Thalassemia (Alpha and Beta)
Basic Overview
Thalassemia is a heterogeneous group of blood disorders affecting the Hemoglobin genes. It is a polygenic disorder that is caused by the Alpha and Beta Globin proteins. The HBA1 & 2 proteins trigger the formation of Globin proteins that are a key unit in the hemoglobin protein (HBA1 Gene). If this does not form right, Hemoglobin will not form correctly and the red blood cells will not be able to carry oxygen efficiently. This disease follows an autosomal recessive pattern, meaning both parents will need to be at least a carrier for you to receive this disease (Image 9). Treatment for this disease depends on the severity but the average person may have to g through blood transfusions, iron supplements, and more. This disease has seen a lot of research towards it and has much better procedures for it. Researchers are currently trying to insert hemoglobin into Bone marrow and they are also trying to find ways to make the hemoglobin into the fetal version as it is weaker (Bajwa & Basit, 2021)
Deeper Explanation
Thalassemia is a heterogeneous group of blood disorders, that affect Hemoglobin and reduce the production of Red Blood Cells. This decrease results in anemia, requiring many blood transfusions to keep the hemoglobin levels steady. Hemoglobin serves as the oxygen-carrying component of red blood cells, and it contains 2 proteins. Alpha and a beta protein. If you cannot produce alpha or beta, you cannot carry sufficient oxygen resulting in anemia and blood transfusions (Bajwa & Basit, 2021). .
There is a clear difference between thalassemia. Alpha Thalassemia is caused by the deletion of the alpha-globin gene, which causes the deletion of the chains(Image 10). This gene has 4 alleles, ranging from least to most severe based on the number of deletions of the allele. If all 4 alleles are lost, you cannot produce any chains, and you start producing excess gamma chains. These are incompatible in life, and you will have to rely on your beta chains. If you lost 1 allele, it is usually masked and not a big issue. On the other hand, Beta Thalassemia is caused by point mutations in the beta-globin gene (Image 10). This gene is broken into 3 categories based on the similarity between both the alleles. A heterozygous mutation results in beta-thalassemia minor which is usually mild and asymptomatic. A homozygous mutation, beta-zero thalassemia results in total deletion of the beta chain and this requires frequent blood transfusions to keep you healthy (Bajwa & Basit, 2021).
If you have a single mutated gene, it is usually mild and asymptomatic causing thalassemia minor but two mutates genes cause thalassemia major (Image 11). Babies born with this swill lose their fetal hemoglobin and gain adult hemoglobin. Excess alpha-globin chains in beta-thalassemia, clump up together causing solid objects that damage the membranes. This also leads to a decrease in red blood cell production. If you have beta thalassemia with a coinheritance of alpha thalassemia, you have a more mild and less severe medical life. Thalassemia is quite complex, as there are over 200 known mutations that can cause this disease. Alpha thalassemia is more prevalent in Asian and African populations, while Beta thalassemia is more popular in the Mediterranean. This could be caused by the food available, environmental conditions, and possible pathogens that are around that area that might affect this disease (Bajwa & Basit, 2021).
Thalassemia has many symptoms, and they depend on the severity of the disease. Symptoms include skin, musculoskeletal, Cardiac, Abdominal, Hepatic, Slow growth rates, and more. These symptoms are quite common and observable, and if you believe that a member of your family heritage has thalassemia and you have these symptoms, you should get it checked. You can easily get it checked by doing things such as checking your Blood count, peripheral blood smear, iron studies, DNA analysis, genetic testing, and more. After getting diagnosed and receiving a result that you have thalassemia, you will be offered different treatments for the severity (Bajwa & Basit, 2021).
For milder versions, you might occasionally need blood transfusions, but for more severe versions, you will need frequent blood transfusions, stem cells, genome editing, gene therapy, and lifestyle changes. Thalassemia minor and major have very large differences, and you should be aware of which form you have before making any decisions (Bajwa & Basit, 2021).
Background:
Alpha vs Beta Thalassemia:
Thalassemia Minor vs Major:
Symptoms & Signs:
Treatments:
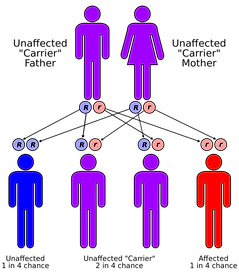
Image 9 : Thalassemia follows an autosomal recessive pattern. Meaning both parents must at least be a carrier for a child to receive it. This is showing in the diagram.
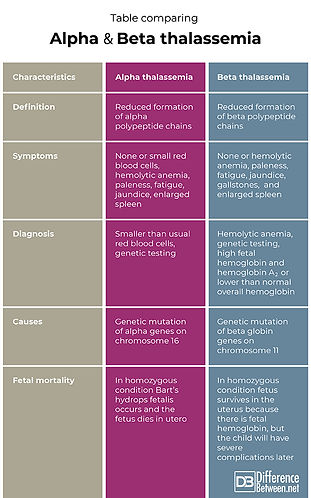
Image 10: Alpha ad Beta Thalassemia are different, as one is more severe than the other. Even then, when comparing them side-to-side, we can find some simple similarities and differences between them.
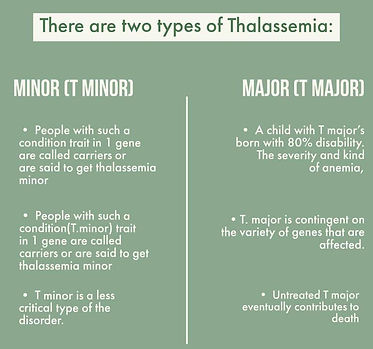
Image 11: This image is differentiating minor and major thalassemia. Thalassemia minor is not very dangerous, and could require some simple things but thalassemia major is much more dangerous.
